BEHAVIORAL SUPPORT SERVICES PROVIDER IN NEVADA
- Fatumata Kaba
- Sep 4, 2025
- 4 min read
Updated: Jan 14
PROMOTING POSITIVE BEHAVIORS AND COMMUNITY INTEGRATION THROUGH PERSONALIZED SUPPORT
Behavioral Support Services in Nevada offer therapeutic interventions and structured support for individuals with disabilities or behavioral health challenges. These services help individuals manage behaviors, develop coping strategies, and improve social interactions, promoting community inclusion and independence. Behavioral Support Services are authorized under Nevada Medicaid Home and Community-Based Services (HCBS) Waiver programs.
1. GOVERNING AGENCIES
Agency: Nevada Department of Health and Human Services (DHHS)
Role: Administers Medicaid waiver funding for Behavioral Support Services and manages provider enrollment, service authorization, and reimbursement.
Agency: Aging and Disability Services Division (ADSD)
Role: Ensures quality standards, service delivery, and compliance for Behavioral Support Services under HCBS waiver programs.
Agency: Centers for Medicare & Medicaid Services (CMS)
Role: Provides federal oversight ensuring Medicaid-funded Behavioral Support Services meet HCBS quality, person-centered planning, and participant protection standards.
2. BEHAVIORAL SUPPORT SERVICES OVERVIEW
Behavioral Support Services aim to address challenging behaviors, develop coping mechanisms, and support emotional well-being through structured interventions.
Approved providers may deliver:
Behavioral Assessment: Comprehensive evaluation of behaviors, triggers, and environmental factors.
Behavioral Intervention Planning: Developing tailored strategies to manage challenging behaviors.
Positive Behavior Support (PBS): Teaching alternative, positive behaviors through reinforcement.
Therapeutic Counseling: Individual or group therapy focusing on behavioral health and emotional regulation.
Crisis Intervention: Immediate support during behavioral emergencies to ensure safety.
Skill Development: Enhancing communication, social interaction, and problem-solving abilities.
Family and Caregiver Training: Educating families on behavioral management and support techniques.
All services are delivered according to the Individualized Service Plan (ISP) and tailored to the participant’s behavioral needs.
3. LICENSING & PROVIDER APPROVAL REQUIREMENTS
Prerequisites:
Register the business entity with the Nevada Secretary of State.
Obtain EIN from the IRS and NPI (Type 2).
Enroll as a Medicaid Waiver Behavioral Support provider via the Nevada Medicaid Provider Enrollment Portal.
Obtain necessary professional licenses (e.g., Board Certified Behavior Analyst (BCBA), Licensed Mental Health Practitioner (LMHP)).
Maintain general liability and professional liability insurance.
Develop policies for behavioral assessment, intervention planning, crisis management, and safety protocols.
Ensure staff meet background checks, health screenings, and relevant behavioral health training requirements.
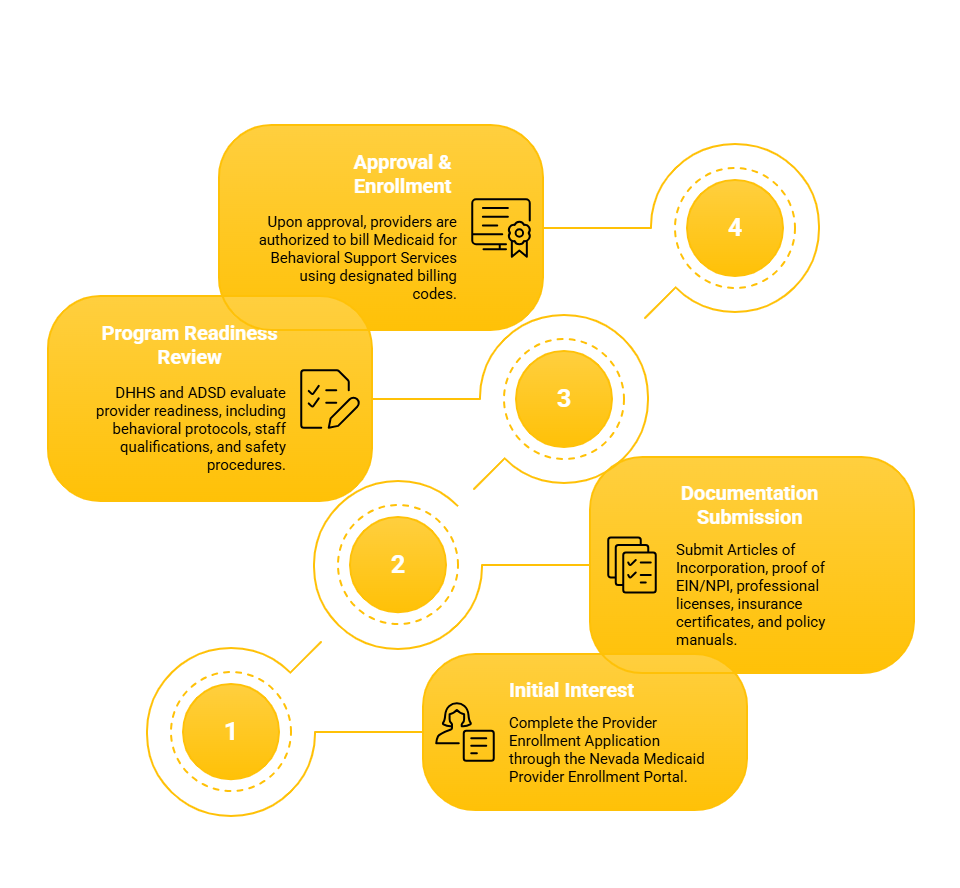
4. NEVADA PROVIDER ENROLLMENT PROCESS
Initial Interest and Application:
Complete the Provider Enrollment Application through the Nevada Medicaid Provider Enrollment Portal for Behavioral Support Services under HCBS waivers.
Application and Documentation Submission:
Submit Articles of Incorporation, proof of EIN/NPI, professional licenses, insurance certificates, and policy manuals.
Program Readiness Review:
DHHS and ADSD evaluate provider readiness, including behavioral protocols, staff qualifications, and safety procedures.
Approval & Medicaid Enrollment:
Upon approval, providers are authorized to bill Medicaid for Behavioral Support Services using designated billing codes.
5. REQUIRED DOCUMENTATION
Articles of Incorporation or Business License (Nevada Secretary of State)
IRS EIN confirmation
NPI confirmation
Professional licenses (e.g., BCBA, LMHP)
Proof of general and professional liability insurance
Behavioral Support Services Policy & Procedure Manual including:
Behavioral assessment, intervention planning, and crisis response protocols
Positive Behavior Support (PBS) and therapeutic intervention guidelines
Staff credentialing, background checks, and training requirements
Documentation standards for progress tracking and Medicaid billing
HIPAA compliance, participant rights, and grievance handling
Crisis management and safety planning protocols
Quality assurance and compliance monitoring
6. STAFFING REQUIREMENTS
Role: Behavioral Support Program Director
Requirements: Master’s degree in psychology, social work, or behavioral sciences; BCBA or LMHP certification; experience in behavioral program supervision.
Role: Behavioral Therapists / BCBA / LMHP
Requirements: State licensure or certification; experience with behavioral assessment and intervention; background clearance.
Role: Direct Support Professionals (DSPs)
Requirements: High school diploma or GED; training in behavioral support techniques; CPR/First Aid certification; background screening.
All staff must complete:
Behavioral intervention and crisis management training
HIPAA compliance and client rights education
De-escalation and positive behavior support training
Annual competency evaluations and professional development
7. MEDICAID WAIVER PROGRAMS
Behavioral Support Services are available under the following Nevada Medicaid Waivers:
Home and Community-Based Waiver for Persons with Intellectual and Developmental Disabilities (HCBS-IDD)
Frail Elderly (FE) Waiver
Physical Disabilities Waiver
Traumatic Brain Injury (TBI) Waiver
Aged and Disabled (AD) Waiver
Services may include:
Behavioral assessment and individualized intervention planning
Crisis intervention and emergency behavioral support
Positive behavior support training and skill development
Family education and caregiver support
Ongoing behavioral monitoring and adjustment
8. TIMELINE TO LAUNCH
Phase: Business Formation and Compliance Preparation
Timeline: 1–2 months
Phase: Staff Hiring, Credentialing, and Program Development
Timeline: 2–3 months
Phase: Nevada Medicaid Provider Enrollment and Readiness Review
Timeline: 60–90 days
Phase: Medicaid Billing Setup and Behavioral Support Service Launch
Timeline: 30–45 days
9. CONTACT INFORMATION
Nevada Department of Health and Human Services (DHHS)
Website: https://dhhs.nv.gov/
Aging and Disability Services Division (ADSD)
Website: https://adsd.nv.gov/
Nevada Medicaid Provider Enrollment Portal
Website: https://www.medicaid.nv.gov/
Centers for Medicare & Medicaid Services (CMS)
Website: https://www.cms.gov/
WAIVER CONSULTING GROUP’S START-UP ASSISTANCE SERVICE — NEVADA BEHAVIORAL SUPPORT SERVICES PROVIDER
WCG supports agencies in launching Medicaid-compliant Behavioral Support Services in Nevada, offering:
Scope of Work:
Business registration, Medicaid enrollment, and licensing assistance
Policy manual development for behavioral assessment and intervention
Staff credentialing, training program templates, and crisis management guidance
Medicaid billing setup and audit-prepared financial management
Branding, website development, and community outreach strategies
Quality assurance systems for behavioral safety and compliance
Collaboration with behavioral health professionals and community agencies
Our Client Portal offers a wealth of resources that you can explore related to various programs and state requirements.
_edited.png)



Comments