CASE MANAGEMENT SERVICES PROVIDER IN SOUTH DAKOTA
- Fatumata Kaba
- Oct 15, 2025
- 3 min read
Updated: Jan 9
GUIDING INDIVIDUALS AND FAMILIES THROUGH PERSONALIZED CARE COORDINATION, GOAL PLANNING, AND COMMUNITY SUPPORT ACCESS
Case Management Services in South Dakota help individuals with disabilities and complex medical needs navigate their support systems, access appropriate services, and maintain stability in home and community settings. These services are available through the CHOICES Waiver, Family Support 360 Waiver, Medically Fragile Waiver, and Long-Term Services and Supports (LTSS) programs. Case Managers act as key liaisons between participants, providers, and state agencies, ensuring services align with each individual’s goals and Medicaid regulations.
1. GOVERNING AGENCIES
Agency: South Dakota Department of Human Services (DHS) – Division of Developmental Disabilities (DDD)
Role: Authorizes and oversees waiver-based case management services, primarily under CHOICES and FS360.
Agency: South Dakota Department of Social Services (DSS) – Division of LTSS
Role: Oversees case management for older adults and medically fragile individuals under LTSS programs.
Agency: Centers for Medicare & Medicaid Services (CMS)**
Role: Establishes federal requirements for person-centered planning, documentation, and HCBS service oversight.
2. CASE MANAGEMENT SERVICES OVERVIEW
Case Management is a targeted support service that includes assessment, planning, service coordination, monitoring, and advocacy on behalf of the participant.
Core responsibilities include:
Initial Assessments and Reassessments
Individualized Service Plan (ISP) Development and Updates
Service Authorization Requests and Monitoring
Referral and Linkage to Medical, Behavioral, and Community Services
Crisis Prevention and Intervention Planning
Documentation and Ongoing Progress Tracking
Facilitating Team Meetings and ISP Reviews
Services must be person-centered, driven by participant choice, and regularly updated.
3. LICENSING & PROVIDER APPROVAL REQUIREMENTS
Prerequisites:
Register your business with the South Dakota Secretary of State
Obtain EIN and Type 2 NPI
Apply through DHS-DDD or DSS as a Medicaid case management provider
Ensure all case managers meet education and experience requirements
Maintain liability and professional insurance coverage
Develop a Case Management Services Policy & Procedure Manual
4. SOUTH DAKOTA PROVIDER ENROLLMENT PROCESS
Step 1: Register your business and obtain EIN/NPI
Step 2: Submit provider application to DHS (for CHOICES, FS360) or DSS (for LTSS/Medically Fragile)
Step 3: Provide sample ISPs, documentation templates, and staff credentials
Step 4: Complete DHS or DSS orientation and compliance readiness review
Step 5: Begin receiving referrals and service authorizations
5. REQUIRED DOCUMENTATION
Articles of Incorporation, EIN, NPI
Proof of insurance (liability/professional)
Staff resumes, background checks, and qualification verifications
Case Management Services Policy & Procedure Manual including:
Intake and person-centered assessment procedures
ISP development and participant goal planning
Contact tracking and monitoring schedules
Critical incident reporting and resolution procedures
HIPAA compliance, documentation standards, and billing protocols
Team meeting facilitation guides and participant rights forms
6. STAFFING REQUIREMENTS
Role: Case Manager / Service Coordinator
Requirements:
Bachelor's degree in human services or related field
At least 1 year of experience with disability services (may vary by program)
Clean background check and valid driver's license
All staff must complete:
Person-centered planning training
HIPAA and participant confidentiality training
Medicaid documentation and billing procedures
Crisis prevention/intervention training
Annual refreshers and quality assurance reviews
7. MEDICAID WAIVER PROGRAMS
Case Management Services are available under:
CHOICES Waiver – For adults with intellectual/developmental disabilities
Family Support 360 Waiver – For children and adults with disabilities living at home
Medically Fragile Waiver – For individuals with complex medical conditions
LTSS Case Management – For seniors and adults needing long-term services and supports
State Plan Targeted Case Management (TCM) – For qualifying populations (varies by age and condition)
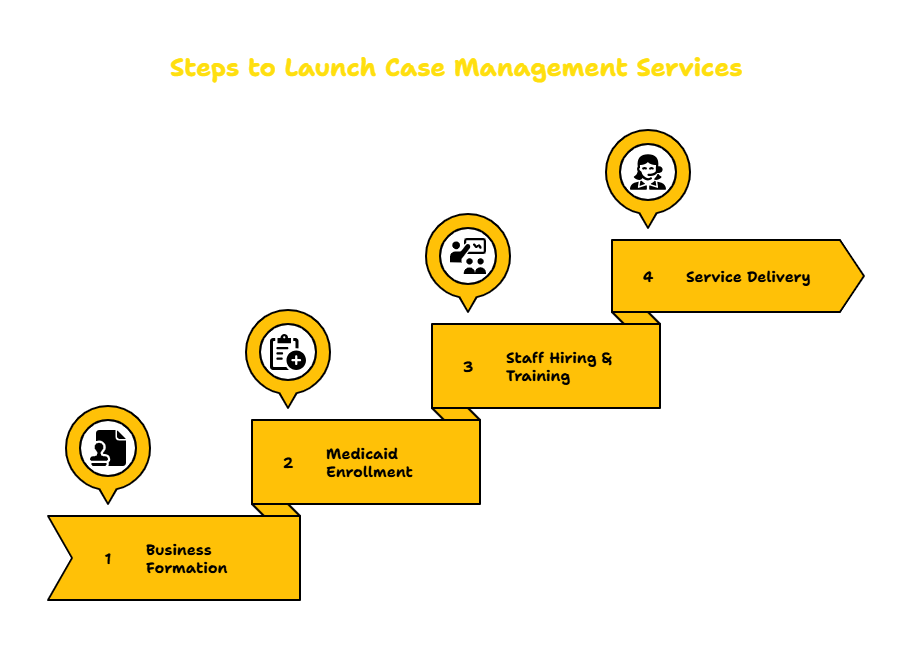
8. TIMELINE TO LAUNCH
Phase: Business Formation & Staffing
Timeline: 1–2 months
Phase: Medicaid Provider Enrollment & Manual Development
Timeline: 2–3 months
Phase: Case Manager Hiring & Training
Timeline: 30–60 days
Phase: Begin Service Delivery
Timeline: After receiving provider approval and service referrals
9. CONTACT INFORMATION
South Dakota Department of Human Services – Division of Developmental Disabilities (DDD)
Website: https://dhs.sd.gov
South Dakota Department of Social Services – LTSS Division
Website: https://dss.sd.gov
Centers for Medicare & Medicaid Services (CMS)
Website: https://www.cms.gov
WAIVER CONSULTING GROUP’S START-UP ASSISTANCE SERVICE — SD CASE MANAGEMENT PROVIDER
WCG helps case managers, human service agencies, and support coordinators launch compliant, person-centered case management operations across South Dakota’s Medicaid waiver landscape.
Scope of Work:
Medicaid enrollment for CHOICES, FS360, and LTSS case management
Policy & Procedure Manual development
ISP templates and person-centered planning tools
Staff credentialing trackers and orientation guides
Service tracking logs and billing documentation templates
HIPAA compliance and team facilitation training
Our Client Portal offers a wealth of resources that you can explore related to various programs and state requirements.
_edited.png)



Comments