CASE MANAGEMENT SERVICES PROVIDER IN RHODE ISLAND
- Fatumata Kaba
- Oct 9, 2025
- 3 min read
Updated: Jan 13
COORDINATING INDIVIDUALIZED CARE PLANS, SUPPORTS, AND RESOURCES TO PROMOTE HOLISTIC WELL-BEING AND INDEPENDENT LIVING
Case Management Services in Rhode Island are Medicaid-funded supports that help individuals navigate health, behavioral, and social service systems. These services are crucial to ensuring that people with disabilities, chronic illnesses, or aging-related needs receive person-centered care aligned with their goals. Case management is authorized under the 1115 Global Waiver, BHDDH DD Waivers, Katie Beckett/TEFRA, and Medicaid State Plan services.
1. GOVERNING AGENCIES
Agency: Rhode Island Executive Office of Health and Human Services (EOHHS)
Role: Manages Medicaid funding, provider enrollment, and service delivery standards.
Agency: Department of Behavioral Healthcare, Developmental Disabilities & Hospitals (BHDDH)
Role: Approves and monitors case managers serving individuals with developmental disabilities.
Agency: Rhode Island Department of Health (RIDOH)**
Role: May regulate case managers working in medical or clinical roles (e.g., RN case managers).
Agency: Centers for Medicare & Medicaid Services (CMS)**
Role: Defines federal requirements for case management under Medicaid HCBS waivers.
2. CASE MANAGEMENT SERVICES OVERVIEW
Case managers help individuals access services, build care teams, and coordinate supports that align with the participant’s goals. Services are person-centered and span across medical, behavioral, housing, education, and employment domains.
Approved providers may deliver:
Assessment & Planning: Conducting person-centered assessments and developing Individualized Service Plans (ISPs).
Referral Coordination: Linking participants to medical, mental health, housing, employment, and community supports.
Care Monitoring: Ensuring services are delivered as planned, and modifying ISPs as needs evolve.
Service Authorization: Submitting documentation to Medicaid or waiver programs for approval.
Crisis & Risk Management: Identifying red flags and facilitating emergency supports.
Documentation: Case notes, visit logs, quarterly progress reviews, and incident reports.
3. LICENSING & PROVIDER APPROVAL REQUIREMENTS
Prerequisites:
Register your business with the RI Secretary of State.
Obtain EIN and Type 2 NPI.
Enroll as a Medicaid Case Management Provider through the EOHHS portal.
For DD waiver case managers, apply and qualify through BHDDH.
Employ or contract qualified case managers with relevant licensure or experience.
Develop a Case Management Services Policy & Procedure Manual addressing planning, compliance, and documentation.
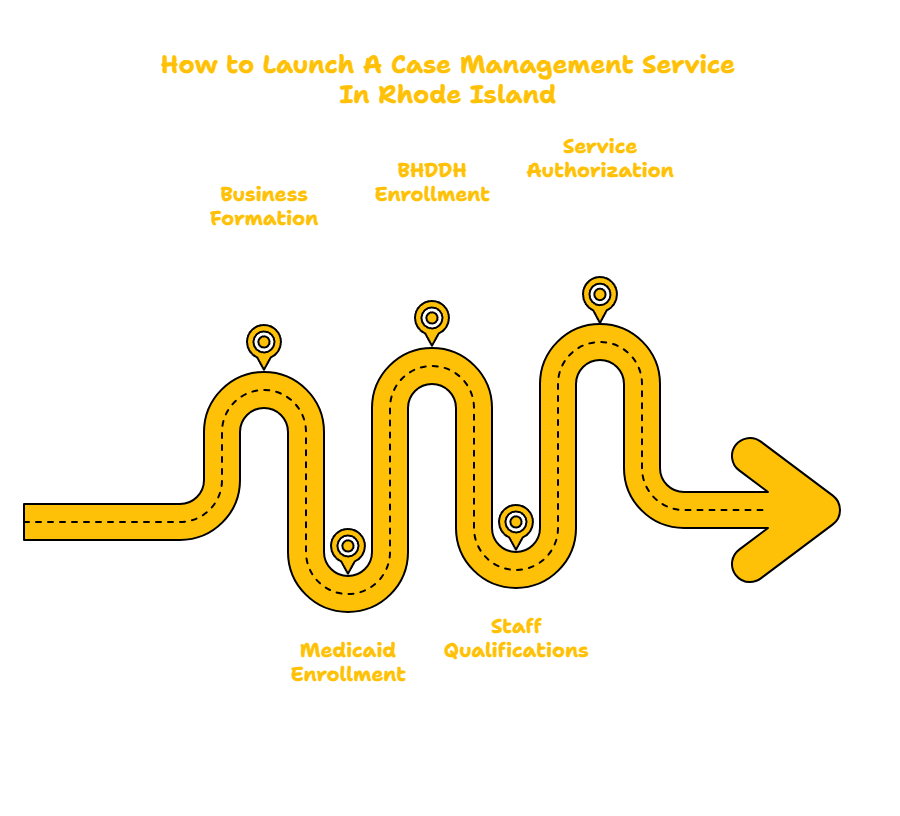
4. RHODE ISLAND PROVIDER ENROLLMENT PROCESS
Step 1: Form your business entity and obtain EIN/NPI.
Step 2: Apply through EOHHS to become a Medicaid case management provider.
Step 3: If serving the IDD population, submit a provider application to BHDDH.
Step 4: Submit staff qualifications, service models, and sample care plans.
Step 5: Begin receiving referrals and authorizations for case management services.
5. REQUIRED DOCUMENTATION
Business registration and Articles of Incorporation
Medicaid provider enrollment and BHDDH approval (if applicable)
NPI confirmation and insurance coverage
Staff licenses (if applicable) and background checks
Case Management Services Policy & Procedure Manual including:
Person-centered planning procedures
ISP development templates
Referral coordination workflows
Risk management and incident response protocols
Documentation and Medicaid billing templates
HIPAA compliance and participant rights documentation
6. STAFFING REQUIREMENTS
Role: Case Manager
Requirements: Degree in human services, social work, or nursing; experience with person-centered planning and system navigation.
Role: RN Case Manager (optional, if serving complex medical needs)
Requirements: Active RN license in RI, knowledge of Medicaid systems.
Role: Case Management Supervisor / Program Director
Requirements: Oversight of ISPs, staff compliance, and quality assurance processes.
All staff must complete:
Person-centered planning and HCBS Settings Rule training
HIPAA and documentation standards
Abuse prevention and crisis de-escalation
Cultural competence and disability rights
Annual reviews and continuing education (as required)
7. MEDICAID WAIVER PROGRAMS
Case Management Services are authorized through:
1115 Global Waiver (HCBS): For individuals with chronic or long-term support needs
BHDDH DD Waivers: Intensive case management for adults with intellectual/developmental disabilities
Katie Beckett/TEFRA: Case coordination for medically fragile children
Medicaid State Plan: For select medical case management services (e.g., hospital discharges, disease management)
8. TIMELINE TO LAUNCH
Phase: Business Formation & Policy Manual Creation
Timeline: 1–2 months
Phase: Medicaid and BHDDH Enrollment (if applicable)
Timeline: 2–3 months
Phase: Staff Hiring & Training
Timeline: 30–60 days
Phase: Participant Assignment & ISP Development
Timeline: Begins once case management authorizations are approved
9. CONTACT INFORMATION
Rhode Island Executive Office of Health and Human Services (EOHHS)
Website: https://eohhs.ri.gov
Department of Behavioral Healthcare, Developmental Disabilities & Hospitals (BHDDH)
Website: https://bhddh.ri.gov
Rhode Island Medicaid Provider Portal
Website: https://www.riproviderportal.org
Rhode Island Department of Health (RIDOH)
Website: https://health.ri.gov
Centers for Medicare & Medicaid Services (CMS)
Website: https://www.cms.gov
WAIVER CONSULTING GROUP’S START-UP ASSISTANCE SERVICE — RHODE ISLAND CASE MANAGEMENT PROVIDER
WCG helps launch and optimize case management services that ensure participants receive person-centered, coordinated care across the lifespan.
Scope of Work:
Medicaid and BHDDH enrollment support
ISP templates and person-centered planning guides
Referral tracking systems and coordination logs
Compliance tools for incident tracking and service monitoring
Policy & Procedure Manual tailored to case management standards
Quality assurance forms and participant satisfaction tools
Our Client Portal offers a wealth of resources that you can explore related to various programs and state requirements.
_edited.png)



Comments