CASE MANAGEMENT SERVICES PROVIDER IN LOUISIANA
- Fatumata Kaba
- Aug 12, 2025
- 4 min read
Updated: Jan 15
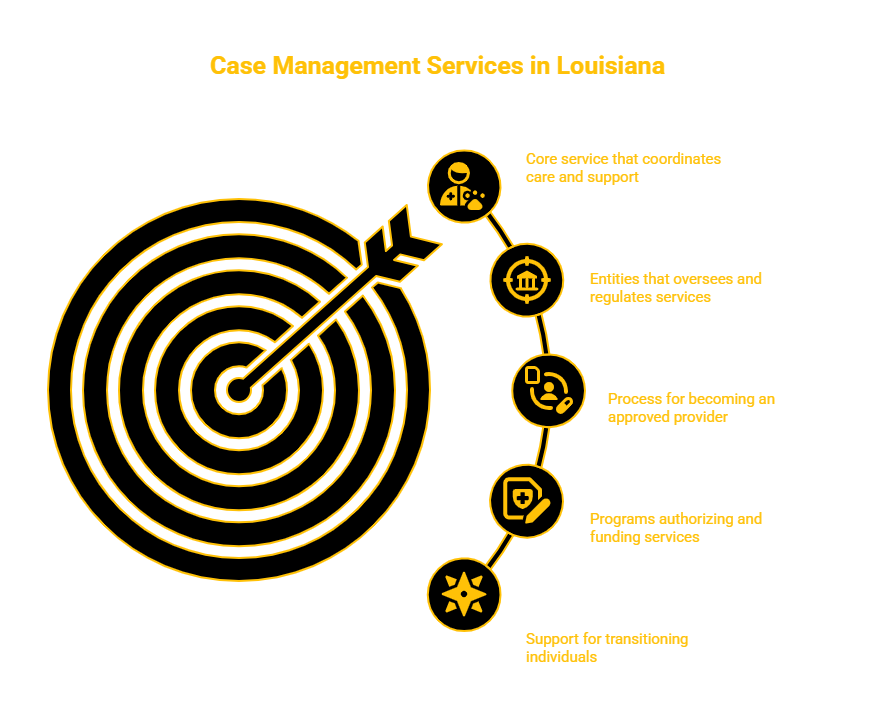
COORDINATING CARE, SERVICES, AND SUPPORT SYSTEMS TO PROMOTE WELL-BEING AND COMMUNITY LIVING
Case Management Services in Louisiana help individuals enrolled in Medicaid and waiver programs access the care and resources they need to live independently. Case managers work directly with participants, families, providers, and state agencies to assess needs, develop individualized care plans, and coordinate service delivery across health, behavioral, and social domains.
1. GOVERNING AGENCIES
Agency: Louisiana Department of Health (LDH) — Office of Aging and Adult Services (OAAS) & Office for Citizens with Developmental Disabilities (OCDD)
Role: Oversees waiver case management guidelines, assigns support coordination agencies, and ensures compliance with person-centered planning
Agency: Centers for Medicare & Medicaid Services (CMS)
Role: Provides federal oversight and ensures case management complies with 1915(c) waiver and person-centered service planning requirements
Agency: Medicaid Management Information System (MMIS) / Molina Medicaid Solutions
Role: Manages enrollment and reimbursement for case management billing
Agency: Managed Care Organizations (MCOs) under Bayou Health
Role: Coordinate with case managers for referrals, authorizations, and data reporting (in specific programs)
2. CASE MANAGEMENT SERVICE OVERVIEW
Case Management (also called Support Coordination) is a comprehensive, person-centered service that includes:
Functional needs assessments and goal setting
Individualized Service Plan (ISP) or Plan of Care (POC) development
Referral to home and community-based services (HCBS)
Coordination with physicians, therapists, and providers
Monitoring of service delivery and participant satisfaction
Critical incident reporting and service plan revision
Advocacy and assistance with transitions (e.g., institutional discharge)
Approved providers support participants in:
Residential Options Waiver (ROW)
Supports Waiver
New Opportunities Waiver (NOW)
Children’s Choice Waiver
Community Choices Waiver (limited case management components)
EPSDT and transition support (for youth aging out of services)
3. LICENSING & PROVIDER APPROVAL REQUIREMENTS
Prerequisites:
Register business with the Louisiana Secretary of State
Obtain IRS EIN and Type 2 NPI
Enroll with Medicaid as a Case Management or Support Coordination provider via the Louisiana Medicaid Provider Enrollment Portal
Apply for waiver-specific designation with LDH (OAAS or OCDD)
Maintain general liability and professional insurance
Employ qualified case managers (e.g., social workers, counselors, or human services staff with experience)
Develop a Case Management Services Policy & Procedure Manual
Ensure HIPAA-compliant documentation and coordination systems
4. PROVIDER ENROLLMENT PROCESS
Step 1: Business and Medicaid Enrollment
Apply through https://www.lamedicaid.com
Submit business documents, staffing plan, and organizational structure
Step 2: Waiver-Specific Approval
Submit an application to LDH OAAS or OCDD to become an approved support coordination agency
Complete background checks, staff credentialing, and service protocols
Step 3: Staff Training and Manual Development
Train staff on person-centered planning, critical incident protocols, and waiver service standards
Implement care planning and documentation tools
Step 4: Referrals and Service Delivery
Receive participant assignments from LDH or MCOs
Begin assessments, service planning, and documentation per waiver rules
5. REQUIRED DOCUMENTATION
Articles of Incorporation or sole proprietorship filing
IRS EIN and NPI documentation
LDH case management designation or waiver program approval
Certificates of insurance
Case Management Services Policy & Procedure Manual, including:
Intake and person-centered planning templates
ISP/POC development forms and service tracking logs
Referral logs and interdisciplinary team coordination forms
Critical incident and grievance reporting policies
Participant rights and informed consent forms
Monthly monitoring and reassessment schedules
Documentation, quality assurance, and billing templates
6. STAFFING REQUIREMENTS
Role: Case Manager / Support Coordinator
Requirements: Bachelor’s degree in social work, psychology, or a related field; 1–2 years’ experience with individuals with disabilities or aging adults; background check clearance
Role: Clinical Supervisor (required for agency model)
Requirements: Licensed social worker or mental health professional; responsible for supervision, service review, and compliance
Training Requirements for All Staff:
HIPAA and participant confidentiality
Person-Centered Planning and waiver rules
Abuse/neglect reporting and incident protocols
Cultural competency and disability rights
Medicaid billing documentation and audit readiness
7. MEDICAID WAIVER & TRANSITION SERVICES
Case Management Services are authorized and reimbursed under:
Residential Options Waiver (ROW)
Supports Waiver
Children’s Choice Waiver
New Opportunities Waiver (NOW)
Community Choices Waiver (limited case management functions)
EPSDT and Money Follows the Person (MFP) transition supports
Approved providers may deliver:
In-home assessments and service coordination
Ongoing case monitoring and documentation
Plan updates and annual reassessments
Coordination of transportation, therapy, home modifications, or direct care services
Transition assistance from institutional care to home/community settings
8. TIMELINE TO LAUNCH
Phase: Business Registration and Staff Hiring
Timeline: 1–2 months
Phase: Medicaid Enrollment and Waiver Approval
Timeline: 60–90 days
Phase: Policy Manual and System Setup
Timeline: 3–4 weeks
Phase: Participant Assignment and Service Delivery
Timeline: Ongoing, based on LDH referrals and waiver enrollment
9. CONTACT INFORMATION
Louisiana Medicaid Provider Enrollment Portal
Website: https://www.lamedicaid.com
Office of Aging and Adult Services (OAAS)
Website: https://ldh.la.gov/page/119
Office for Citizens with Developmental Disabilities (OCDD)
Website: https://ldh.la.gov/page/121
Louisiana Department of Health (LDH)
Website: https://ldh.la.gov
WAIVER CONSULTING GROUP’S START-UP ASSISTANCE SERVICE — LOUISIANA CASE MANAGEMENT PROVIDER
We help qualified professionals and agencies launch Medicaid-approved case management services for Louisiana HCBS waiver participants.
Scope of Work:
Medicaid enrollment and waiver designation process
Policy & Procedure Manual development for service coordination
Intake and care planning templates
Compliance checklists for documentation, billing, and audit prep
Staff training logs and credentialing support
Referral outreach and LDH partnership strategies
Our Client Portal offers a wealth of resources that you can explore related to various programs and state requirements.
_edited.png)



Comments